In this article
Acne is a relatively common skin condition that has been linked to a variety of factors and especially hormones such as testosterone (T).
That is because the sebum-producing glands in the skin are particularly sensitive to T and other androgens (male sex hormones).
The glands respond to androgens by increasing sebum production and creating conditions for inflammation, ultimately leading to the occurrence of pimples and cysts typical for acne.
Thus, sudden increases in androgens levels related to age, physiological processes, diseases, or steroid abuse may contribute to acne breakouts. Genetic predisposition, such as a higher sensitivity of the sebaceous glands to androgens, also plays a major role.
Even medications such as legal testosterone replacement therapy (TRT) can potentially lead to acne in individuals with predispositions. However, acne breakouts caused by TRT are rare and usually mild. They can also be addressed quickly when the TRT is monitored by an experienced medical professional.
Keep reading to discover how exactly testosterone and TRT are related to acne, what the most common risk factors are, and how to manage and prevent it.
Does testosterone cause acne?
Research suggests that testosterone is associated with the occurrence of acne because as T levels increase, there is a concurrent increase in the secretion of sebum.
As sebaceous glands start producing too much sebum, they may get clogged, which creates conditions for increased bacterial growth inside their follicles. As a result, the follicles of the gland get inflamed, causing typical signs of acne such as pimples.
Sometimes, the inflammation can occur deep within the skin’s sebaceous glands, leading to the formation of cysts. Similar to other types of acne, cystic acne is also related to inflammation of the sebaceous glands, which may be associated with androgen levels.
Due to the link between androgen levels and the occurrence of acne, many individuals also refer to the condition as “hormonal acne.”
However, the condition has a complex pathogenesis. Thus, the role of androgenic hormones is just one of the two main factors that act in combination and lead to acne.
Namely, they include increased sebum production (potentially related to androgens) as well as bacterial overgrowth. Therefore attempting to differentiate between hormonal acne and “bacterial acne” would be inappropriate.
Interestingly, research suggests that individuals (both men and women) suffering from acne have normal serum testosterone levels. Moreover, the studies suggest there is only a slight correlation between individual testosterone levels and acne severity.
Instead, the evidence reveals that the local overproduction of active androgens may play a much more significant role in the pathogenesis of this condition. Acne patients may actually produce higher levels of testosterone and other androgens locally – in the skin and the sebaceous glands.
More specifically, the activity of sebaceous glands is heavily influenced by the levels of an androgen called 5α-dihydrotestosterone (5α-DHT).
5α-DHT is produced locally by the 5α-reductase type I enzyme found in the cells of the sebaceous glands. More specifically, the 5α-reductase converts testosterone from the serum into 5α-DHT that acts locally on the skin and the glands.
5α-DHT has a much stronger affinity for the androgen receptors in the sebaceous glands than T and provides a significant stimulus for sebum production.
The activity of the 5α-DHT found in sebaceous glands, as well as the sensitivity of their androgen receptors, may be higher in acne patients, potentially explaining why they experience skin problems even when having normal T levels.
Individuals suffering from low T usually do not experience acne vulgaris. However, receiving treatment for low T, such as in the form of TRT, may increase the risk of acne, especially in sensitive individuals and those taking inappropriately excessive doses of the medication.
Inappropriate TRT dosage may also lead to other negative consequences, such as experiencing difficulty urinating, increasing levels of daytime sleepiness, and fatigue due to the high serum T levels.
Can testosterone therapy cause acne?
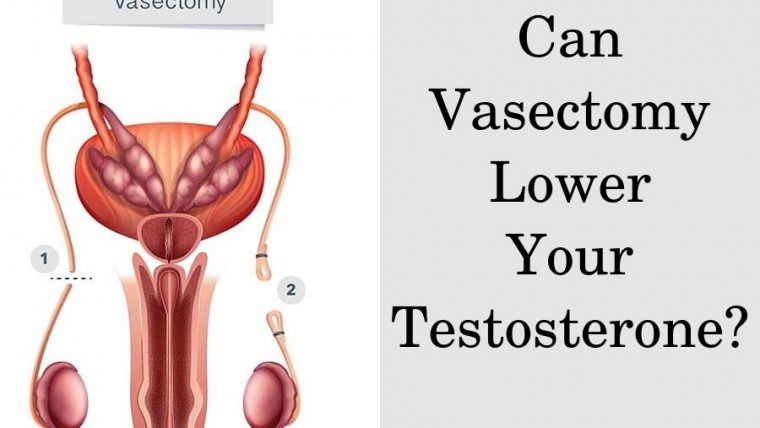
According to the Clinical Practice Guideline of the Endocrine Society for TRT in men, oily skin and acne are some of the side effects which may occur due to testosterone therapy.
Other proven side effects of TRT in men included increased red blood cell levels, suppressed testicular function, and infertility. It is possible that TRT could lead to water retention.
Furthermore, a meta-analysis of testosterone therapy effects in postmenopausal women with hypoactive sexual desire disorder (HSDD) reports that the therapy was also associated with an increased incidence of acne.
Research in female-to-male (FtM) transgender patients also reports that the incidence of acne increased from 6.3% to 31.1% after the initiation of masculinization therapy with testosterone. Studies in FtM patients also report that acne severity increases in individuals who already had the problem before starting the therapy.
Unfortunately, there aren’t studies in men to report if starting TRT worsens pre-existing acne in males. Nevertheless, research reveals that testosterone therapy can increase the risk of acne in both men and women.
This is likely due to the fact that TRT leads to an increase in serum T levels, and once the hormone reaches the skin, it can get transformed to 5α-DHT and interact with the sebum production by sebaceous glands.
However, whether a person on TRT experiences acne will also depend on the local expression of the 5α-reductase enzyme and the sensitivity of the androgen receptors found in sebaceous glands.
Thus, increased testosterone will always cause acne, and its occurrence depends on the susceptibility of the patient. As evident from the data on FtM patients, supraphysiological doses of testosterone therapy also increase the risk of acne.
Currently, there is no evidence on whether the risk of acne varies between different forms of TRT. However, some studies suggest that transdermal testosterone may lead to a higher increase in 5α-DHT levels compared to testosterone injections. Therefore, testosterone injections may pose a lower risk for acne compared to other formulations.
In comparison, dietary supplements labeled as testosterone boosters cannot reliably increase serum T levels or upregulate the sensitivity of the sebaceous glands to androgens. In fact, some studies suggest that roughly 10% of the ingredients in most common T boosters may have a negative effect on male hormones. Therefore, testosterone-boosting supplements can’t cause acne.
Where does testosterone acne usually appear?
Acne Vulgaris appears to affect specific skin areas, regardless of whether it is associated with TRT or not. These areas are commonly referred to as sebaceous gland-rich areas as they have a high concentration of oil glands.
According to research, the main areas include the face, upper arms, chest, and back. Acne often occurs on the face, particularly on the forehead, nose, chin, and jawline.
Areas such as the chest, upper back, shoulders, and upper arms are also common sites for acne breakouts related to hormonal imbalances and elevated testosterone levels.
Certain skin areas that are rich in sebaceous glands may be affected more severely than others also because of variations in androgen receptor sensitivity and 5α-reductase enzyme activity in these zones.
Is back acne a sign of high testosterone?
Having truncal acne, including back acne, does not necessarily indicate high testosterone or testosterone use.
That’s because the occurrence of acne depends primarily on individual sensitivity rather than serum T. Patients suffering from this skin condition usually have normal testosterone levels, regardless of which area of the body is affected.
However, back acne has become notorious as a sign of high androgen levels, especially in individuals abusing anabolic steroids. The occurrence of back acne in bodybuilders is also often referred to as “bodybuilding acne” or “bacne.”
Indeed, anabolic steroid abuse has been reported to cause acne lesions on the face and the body, affecting as much as 50% of users.
Apart from acne vulgaris, researchers have reported the occurrence of more severe types as well, such as acne conglobata and acne fulminans, both of which may affect the back, other parts of the body, and the face.
To effectively address back acne resulting from steroid abuse, the foremost step is to promptly discontinue their usage. Additionally, strategies commonly employed for managing facial acne will also yield comparable effects for alleviating back acne.
How long does testosterone acne last?
Acne Vulgaris is a self-limiting condition which means it tends to resolve with time. Unfortunately, data from males taking TRT for hypogonadism is scarce and does not report how long testosterone-related acne may persist.
The data from FtM patients reveals that acne incidence increases most dramatically during the first 4 months of testosterone treatment, especially in areas of the trunk.
The severity increased over the first six months but then started to decrease until the end of the first year. Thus, acne may subside in some but not all patients on TRT.
Ultimately, the data suggest that some patients may have to deal with acne for as long as they receive testosterone therapy.
How to treat acne from testosterone
One of the most obvious options to manage acne caused by testosterone therapy is to lower the dose of complete cease TRT.
However, this may not be a viable choice for men with hypogonadism as the symptoms of low T, such as sexual dysfunction, muscle loss, and depressive mood, will likely recur.
Instead, various medications and over-the-counter (OTC) remedies may help manage the problem. Some of the most common over-the-counter remedies include topical solutions containing:
- benzoyl peroxide
- salicylic acid
- azelaic acid
- topical retinoids
Benzoyl peroxide is present in a wide variety of face washes and cleansers which can be applied to all parts of the body affected by acne. Research suggests that it is significantly more effective than placebo for improving acne symptoms.
Studies also suggest that salicylic acid washes, azelaic acid washes, and topical retinoids have comparable effectiveness to benzoyl peroxide.
Prescription medications for managing acne include:
- isotretinoin
- antibiotics (topical and oral)
- spironolactone
- contraceptives
Also, isotretinoin helps reduce the excessive production of sebum to prevent the clogging of hair follicles. It may also help to inhibit the formation of these comedones by regulating the keratinization process.
Further, isotretinoin has been shown to have some antibacterial properties, specifically against the bacteria Propionibacterium acnes, which is commonly found on the skin and can contribute to the development of acne.
In addition, several topical and oral antibiotics can also target Propionibacterium acnes and may help reduce acne severity. Examples include trimethoprim/sulfamethoxazole, macrolides, and tetracyclines.
Spironolactone and oral estrogens (contraceptives) are potent androgen-blockers, which can help reduce the sebum-promoting effects of testosterone and DHT and result in significant improvement of acne symptoms.
However, due to the risk of serious side effects, including sexual dysfunction and gynecomastia in men, spironolactone and oral contraceptives are recommended for treating acne only in females.
How to prevent acne while on testosterone
Patients who are already on TRT or considering TRT for managing their symptoms should consider the following factors that can help minimize the risk of acne:
- Use only legal TRT
- Appropriate skin-care routine and products
- Appropriate shaving routine
- Avoid touching your face
- Healthy lifestyle and smoking cessation
The best way to prevent the occurrence of acne while on testosterone is to receive legal TRT from an experienced medical doctor who will monitor your therapy for effectiveness and early signs of side effects.
By titrating the dose of TRT carefully, your physician can help minimize the occurrence of acne or completely prevent breakouts, as well as prevent other adverse reactions.
In addition, all patients are advised to follow a consistent skincare routine to further reduce their risk of acne breakouts. Maintaining appropriate skin care helps by preventing excess sebum accumulation and bacterial overgrowth.
For example, it’s important to use a gentle cleanser to keep your skin clean, but be careful not to scrub too vigorously as it can irritate and worsen acne.
Keep in mind to moisturize regularly with lightweight, oil-free moisturizers, even if your skin feels oily, as excessive drying can trigger increased oil production.
Additionally, refrain from touching your face to prevent transferring oils, dirt, and bacteria that can aggravate acne. Picking or popping pimples should also be avoided, as this can lead to inflammation, scarring, and prolonged healing time.
Men should also pay special attention when shaving by using a clean, sharp razor and shaving in the direction of hair growth to minimize irritation and razor bumps.
A healthy lifestyle and smoking cessation may also help reduce the risk of acne breakouts as well as their severity. One meta-analysis of 17 observational studies reports that smoking was associated with a higher risk of acne in adults but not in adolescents.
Cigarette smoke contains various components that can impact the skin, such as nicotine, which has hyperkeratosis-inducing properties. Other substances in cigarette smoke can stimulate inflammatory pathways and potentially aggravate acne.