In this article
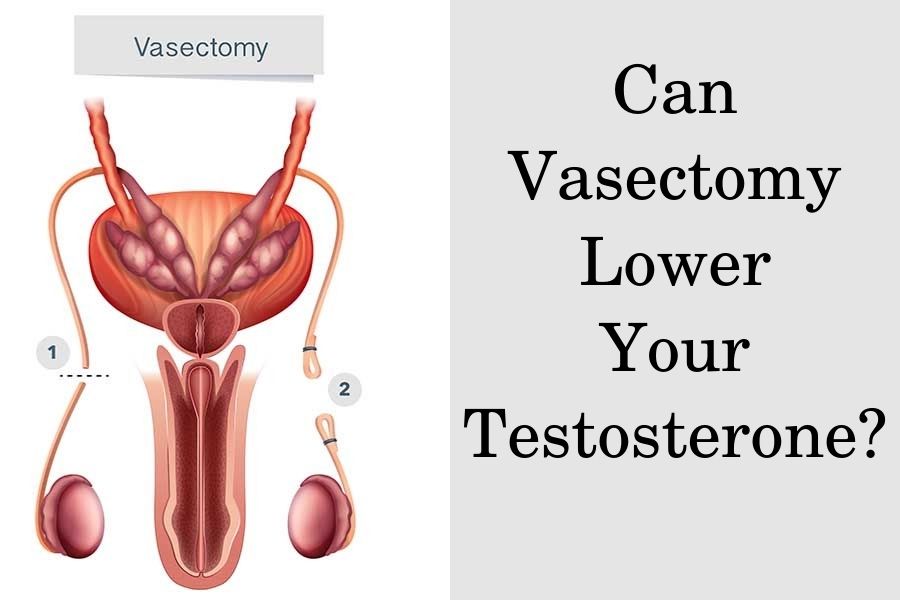
Many men considering vasectomy are worried about their natural testosterone (T) production.
That’s because the testicles are the main organs that produce testosterone in males, and vasectomy involves incising and sealing their sperm ducts.
Yet, vasectomy does not affect the blood supply to the testicles, and the production of testosterone that gets transported to the rest of your body via blood circulation.
Unfortunately, your testosterone production may be affected due to other testicular problems, which sometimes also require surgical interventions.
Testicular diseases that can lead to low T and primary hypogonadism include genetic conditions (Klinefelter’s), testicular cancer and its treatment, cryptorchidism, orchitis (mumps), hemochromatosis, and testicular injury.
What happens during a vasectomy procedure?
During a vasectomy, a surgeon makes a tiny incision on the scrotum in order to reach the ducts that transport semen out of the testicles during ejaculation.
These ducts are called vasa deferentia, and during the procedure, they are cut, separated, and sealed to prevent the passage of sperm.
If a vass defference is cut but not appropriately sealed, there is a chance that the ends can grow back together and become reattached.
The whole procedure usually takes less than 30 minutes, and there is no need for a hospital stay. Usually, you can resume sexual function without any or only minimal discomfort within a week of the procedure.
However, it may take up to 3 months until the procedure reaches maximum effectiveness in reducing male fertility completely. Studies report that after this initial period, effectiveness reaches 99%.
What happens to testicles after vasectomy?
The testicles, as well as their blood supply and innervation, are not affected during the procedure, so their function remains unaffected. Thus there shouldn’t be any changes in their size, such as testicular shrinkage after a vasectomy.
Yet, there is mixed evidence on the effect of the intervention on sexual health. Some studies report that about 6% of vasectomized patients may experience a decrease in libido.
On the other hand, trials are reporting that men who have undergone vasectomy have sexual intercourse more frequently as well as increased sexual desire and satisfaction.
No cases of surgery-related erectile dysfunction were reported
Researchers who have investigated whether or not the procedure may affect erections also report that there haven’t been cases of somatic erectile dysfunction.
Yet, there were cases of psychological erectile dysfunction in men who may have had the decision to undergo vasectomy imposed upon them by their partner.
In such cases, men may opt-out for vasectomy reversal, which has up to a 75% success rate if performed within 3 years of the initial surgery.
Long-term adverse reactions related to vasectomy may include post-vasectomy pain syndrome. The condition may affect about 14% of all patients, and in rare cases, it is severe, debilitating, and reduces those individuals’ quality of life.
Does a vasectomy reduce testosterone?
Currently, there is no evidence that a successful vasectomy may have any side effects on testosterone production by the testicles. Similarly, vasectomy reversal also should not affect testosterone production.
Therefore, your T levels will not drop unless there has been a complication during the surgery that affects your testicles. Levels of some male sex hormones may even rise in the long term after a vasectomy.
One long-term trial reported that men who had undergone vasectomy 10-19 years before the study had higher dihydrotestosterone (DHT) levels than age-matched controls.
Those who had undergone the procedure more than 20 years prior to the investigation also had higher T levels.
Do you need testosterone therapy after a vasectomy?
Since vasectomy is not likely to affect the function of your testicles, there is no need to undergo testosterone replacement therapy (TRT) following the procedure.
Yet you can continue taking TRT after the surgery in case you have another condition that affects your natural testosterone production.
Testosterone treatment cannot reverse a vasectomy or reduce its success rate
In fact, TRT may also lead to infertility since the therapy can suppress the endogenous testosterone production that’s required for the development of functional sperm in the testicles.
Therefore, TRT may increase the success rate of vasectomy during the first 3 months after the surgery as there is still some chance for being fertile during that period.
In case you decide to undergo a vasectomy reversal, undergoing TRT at the same time may reduce your chances of successfully restoring your fertility. However, discontinuing testosterone therapy before the reversal has been shown to successfully restore fertility in some patients.
What testicular disorders can affect testosterone?
Some of the testicular conditions that may affect the function of the testes and impair testosterone production include:
- inflammation of the testes (orchitis)
- testicular cancer and related treatment (incl surgical removal)
- testicular injury
Orchitis may occur due to viral or bacterial infection. The most common viral orchitis is mumps which is a vaccine-preventable condition. Bacterial orchitis usually occurs due to sexually transmitted diseases (gonorrhea, chlamydia) or urinary tract problems.
In rare cases, the condition can lead to shrinkage of the affected testicles or even death of testicular tissue. In such cases, the testes may not be able to produce testosterone and functional semen, which leads to sterility.
Testicular cancer usually affects one rather than both testicles. The affected testis is always removed entirely in a procedure called orchiectomy. Depending on the stage of cancer, the patient may also require radiotherapy and chemotherapy.
Although one remaining testis is sufficient to maintain testosterone production and fertility, testicular tissue is extremely susceptible to radiotherapy and chemotherapy. The additional treatment may damage the remaining testicle, leading to infertility and low T.
Orchiectomy of one or both testicles may also be performed due to severe testicular trauma or injury that has led to the death of most of the testicular tissue. If testicular torsion is not treated within 6 hours of the event, it also leads to the death of the testicle and requires surgical removal.
If the function of both testicles has been affected or they have been removed, it leads to the development of low testosterone and hypogonadism. This warrants treatment via testosterone replacement therapy.
TRT can help restore the normal testosterone levels in your body and alleviate the symptoms of low T such as muscle loss, weight gain, chronic fatigue, erectile dysfunction, lack of libido, and depression.