In this article
Sleep is essential to human life as it plays a crucial role in maintaining physical and metabolic health. During sleep, the body regulates vital processes such as tissue recovery, body temperature, and hormonal synthesis.
One of the hormones produced primarily during sleep is the human growth hormone (HGH). In fact, HGH has a pulsatile secretion that coincides with specific phases of your sleep throughout the night.
Moreover, patients suffering from growth hormone deficiency (GHD) may be more likely to experience sleep disturbances and reduced sleep quality.
Furthermore, GHD patients also often complain of weight gain, decreased muscle mass, and lack of energy, which, combined with sleep problems, can significantly decrease a person’s quality of life.
On the other hand, scientists are still investigating whether sleep problems and insomnia may suppress HGH synthesis as well and lead to symptoms.
When is growth hormone released during sleep?
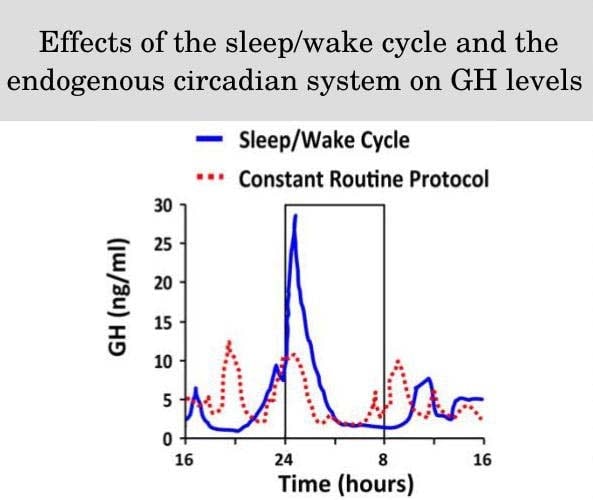
Scientists consider sleep as one of the major regulators of growth hormone synthesis, alongside the circadian rhythm and regulatory hormones.
In fact, several studies report that HGH levels increase during sleep, with the major increase occurring soon after sleep onset, irrespective of the time of day that sleep takes place.
Furthermore, the researchers reported that the peaks in HGH tended to occur at regular intervals of about 2 hours during a regular night’s sleep and coincide with slow-wave sleep phases.
The circadian rhythm also plays a role in HGH synthesis. Trials that involved short-term sleep restriction by delaying bedtime until 1 am reported that there was a pre-sleep peak in HGH, which was likely related to the person’s circadian rhythm.
Nevertheless, the rest of the HGH peaks occurred right after sleep onset, and coincided with the phases of slow-wave sleep. It’s important to note that they were lower compared to the HGH peaks, which occur during regular non-restricted sleep.
Slow-wave sleep is also known as deep sleep or stage 3 sleep, and it usually occurs in between light sleep (stages 1 and 2) and REM sleep (stage 4).
During stage 3 or slow-wave sleep, the body is relaxed, breathing slows down, and heart rate decreases. This is the phase that is considered as most important for physical recovery and restoration.
On the other hand, REM (rapid-eye movement) sleep is the phase when dreams occur, and it is considered to play a major role in mental recovery.
Yet, HGH is not released during REM sleep, and depriving individuals of this phase doesn’t lower growth hormone levels although it may lead to other negative effects such as memory problems.
Researchers point out that the highest release of HGH in healthy people usually occurs within 30 minutes of sleep onset. This coincides with the first and longest phase of slow-wave sleep, which occurs during the first sleep cycle and lasts for about 45-90 minutes.
It’s important to note that human sleep is structured in such a way that every next sleep cycle involves a shorter phase 3 (slow-wave sleep) and a longer phase 4 (REM).
Furthermore, the last cycle before waking up usually does not involve any slow-wave sleep at all. About 70% of the pulses during sleep coincide with slow-wave sleep phases.
Interestingly, short-term sleep deprivation does not appear to have a negative effect on HGH synthesis. Studies report that HGH peaks were lower during a sleepless night but significantly increased in frequency and amplitude during the next day, even though the subjects were awake. The evidence is less conclusive regarding the effects of chronic insomnia on HGH secretion.
Slow-wave sleep and HGH
Despite the fact that HGH is produced primarily during slow-wave sleep, the application of sound disruption during this phase doesn’t diminish HGH synthesis.
Instead, scientists suggest that HGH peaks and slow-wave sleep may coincide because they are both stimulated by factors such as growth hormone-releasing hormone (GHRH) and ghrelin.
Animal studies suggest that the release of GHRH stimulates various sleep-regulatory neurons in the brain and leads to an increase in slow-wave sleep.
Therefore, the episodic release of GHRH while sleeping stimulates the peaks in growth hormone but also regulates the occurrence of slow-wave sleep.
Furthermore, ghrelin levels are also increased during the early part of sleep and this response is blunted when sleep does not occur.
Repetitive intravenous infusion of ghrelin increases both growth hormone levels and slow-wave sleep. At the same time, ghrelin decreases REM sleep. Thus, the increase in ghrelin during early sleep may also be a major contributing factor to the concomitant increase in HGH levels.
Can you increase HGH levels during sleep?
If you want to increase your HGH levels during sleep, you should focus on several potentially effective strategies, such as optimizing your circadian rhythm, avoiding factors that can shorten or prevent slow-wave sleep, and maximizing GHRH/ghrelin production.
In order to optimize both your circadian rhythm and your sleep quality, it is crucial to have a regular sleep schedule. Going to sleep at regular times daily will help your body fall asleep faster and consistently achieve higher HGH peaks during sleep.
Research also suggests that avoiding late dinners and nighttime eating soon before bed may optimize ghrelin secretion and thus improve HGH levels during sleep.
One study showed that individuals who had night eating syndrome had lower ghrelin and HGH levels compared to healthy controls. Therefore, making sure that you are not consuming any food for at least a couple of hours before going to bed may help improve HGH levels during sleep.
Fasting is also known to induce a release in HGH levels, and the duration of fasting correlates with the increase in total HGH synthesis. Diets such as intermittent fasting can increase HGH but may also hamper its anabolic functions by lowering the production of IGF-1.
Factors that prevent or shorten slow-wave sleep may also disrupt the normal release of HGH since both events usually coincide while sleeping. Thus, preventing factors with negative effects on slow-wave sleep may be beneficial for HGH.
For example, consuming caffeine close to bedtime may disrupt and shorten slow-wave sleep, which in theory, may also be associated with reduced HGH synthesis. While there is no research on the effect of caffeine on HGH levels, avoiding stimulants close to bedtime may have benefits for sleep quality.
Ensuring optimal melatonin synthesis by avoiding blue light close to bedtime and taking exogenous melatonin is another common strategy for improving sleep. However, the evidence is inconsistent regarding the effect of melatonin on HGH synthesis during sleep.
Some trials suggest that melatonin supplementation may improve HGH synthesis, while other researchers report no effect at all. It’s important to note that both peak and area under the curve HGH levels increased when taking exogenous melatonin.
Yet, the evidence consistently shows that melatonin supplementation reduces the duration of slow-wave sleep.
Studies also report that HGH may also peek during daytime sleep, such as when taking a nap. The scientists reported that taking a nap in the PM appears to induce a higher release of HGH compared to a nap before noon.
How can HGH therapy affect your sleep?
Patients with GHD often suffer from reduced energy levels and fatigue. And some of them reported that the quality of their sleep had worsened. One of the reasons may be the disruption of the normal sleep cycle.
GHD patients due to pituitary damage had an increase in slow-wave sleep, which was likely due to a lack of negative feedback from the gland and a consequent increase in GHRH synthesis in the hypothalamus.
On the other hand, patients spent less time in slow-wave sleep if they had GHD due to hypothalamic dysfunction and lack of GHRH.
The fact that the etiology of GHD may impact sleep differently may also explain why the current evidence is inconsistent regarding the benefits of exogenous growth hormone on sleep in those patients. Currently, exogenous HGH therapy is the only FDA-approved therapy for managing GHD.
Yet, some studies show that HGH therapy may also improve sleep quality in patients with GHD, while others report no effect of growth hormone injection on sleep disorders and daytime sleepiness. The trials that suggest a positive effect of HGH report that the improvements tend to occur within 3 months of therapy.
Those treated with HGH also experienced a slight reduction in total sleeping time. That may be because the increase in serum HGH provides negative feedback on the hypothalamus.
In turn, this reduces GHRH and decreases the length of the slow-wave sleep phases. As a result, studies report that HGH also increases REM sleep. Despite the fact that HGH may shorten sleep length, there are no reports of HGH therapy causing insomnia.
Since the majority of growth hormone is released during sleep, experts recommend taking HGH injections in the evening rather than the morning. Taking the medication before bed also had a lower risk of side effects, such as reduced insulin sensitivity.
That’s because HGH’s half-life is about 3.5 hours, which allows serum growth hormone levels to decrease until the next morning and prevents interaction with insulin.
Can HGH treatment cause sleep apnea?
Obstructive sleep apnea (OSA) is one of the most common forms of sleep-disordered breathing (SBD).
There may be an association between HGH levels and the occurrence of OSA. More specifically, having extremely high serum growth hormone levels, such as in acromegaly, has been associated with sleep apnea.
Studies also report that acromegaly treatment which results in reducing serum HGH levels may also help improve OSA symptoms. The exact cause of OSA in acromegaly is not yet fully understood.
Yet, studies report that the elevated IGF-1 levels, which are a consequence of the high HGH levels, may play a role by interacting with the respiratory centers in the brain and causing another form of sleep apnea called central sleep apnea (CSA).
Despite these observations, exogenous HGH therapy does not lead to any form of sleep apnea, including OSA, in patients with GHD. Furthermore, HGH injections did not aggravate already existing OSA and even improved the quality of life in these patients.
It is unknown if OSA itself can lead to low HGH synthesis. Some studies suggest that OSA reduces the time spent in slow-wave sleep, which is also associated with a blunted HGH secretion, but more research is needed to confirm such a relationship.